“Reduce call volume and improve policyholder satisfaction with Automated Insurance Claim Status Updates that proactively inform customers and free up your team for complex issues.”
The phone rings. Again. Your call center agent picks up, ready for the inevitable question: “I’m just calling to check on the status of my claim.”
Sound familiar? For P&C insurance carriers, this question is the drumbeat of daily operations. It’s a constant, relentless flood of inbound calls from anxious policyholders who want to know what’s happening. Each call represents a moment of friction, a point of anxiety for your customer, and a tangible cost to your business. While your team repeatedly answers the same question, the actual work of processing claims slows down. It’s a vicious cycle of reactive communication that drains resources, frustrates customers, and hurts your bottom line.
But what if you could break that cycle? What if you could answer your policyholder’s question before they even think about asking it?
This is the power of a proactive communication strategy, driven by automated insurance claim status updates. It’s about transforming your claims process from a reactive, costly system into a proactive, efficient, and customer-centric operation. By leveraging a dedicated AI Claims Assistant, you can not only silence the endless ringing of the phone but also create a policyholder experience that builds trust, loyalty, and satisfaction. It’s time to stop playing defense and start proactively managing the conversation.
The Crushing Cost of the Status Quo
The traditional, reactive approach to claims communication is more than just an annoyance; it’s a significant operational and financial burden. Let’s break down the real-world impact of forcing your policyholders to call you for updates.
The Financial Drain of High Call Volume
First and foremost, inbound calls cost money—a lot of it. Consider the infrastructure required to handle thousands of “where’s my claim?” calls every month.
- Staffing Costs: You need a team of customer service representatives dedicated to answering these calls. This involves salaries, benefits, training, and overhead. A single, fully-loaded call center agent can cost a company upwards of $50,000 to $70,000 annually. If a significant portion of their day is spent providing simple status updates, that’s a massive expense for a low-value, repetitive task.
- Operational Inefficiency: Every minute an agent spends on the phone is a minute they can’t spend on more complex issues. Industry benchmarks often place the cost of a single inbound customer service call anywhere from $6 to over $20, depending on the complexity and duration. Even at the low end, if you’re fielding 10,000 status-check calls a month, that’s a direct operational cost of at least $60,000—or nearly three-quarters of a million dollars a year—just to tell people information that should be readily available.
- Adjuster Distractions: The burden doesn’t just fall on the call center. Frustrated policyholders who can’t get through or want to speak directly to the source will call their assigned adjuster. This is a catastrophic drain on your most valuable claims resource. When experienced adjusters are pulled away from investigating, evaluating, negotiating, and settling claims to provide a simple status update, the entire claims pipeline grinds to a halt. You’re paying a skilled professional a high salary to do the work of an automated message. It’s the definition of inefficiency.
The “Anxiety Gap”: A Failing Policyholder Experience
Beyond the direct financial costs, the reactive model creates a terrible customer experience. When a policyholder files a claim, they are often in crisis. Their car has been wrecked, their home has been damaged, or their business has been interrupted. They are stressed, vulnerable, and uncertain about the future.
In this state, silence is deafening.
We call this the “anxiety gap”—the space between when the policyholder expects an update and when they actually receive one. Every day that passes without communication, their anxiety grows. They start to wonder:
- Did they receive my claim?
- Is someone working on it?
- Did I fill out the forms correctly?
- When will I get my car fixed?
- When will we be able to move back into our house?
This uncertainty forces them to pick up the phone. They aren’t calling because they want to; they are calling because the lack of information has become unbearable. The experience of navigating a phone tree, waiting on hold for 15 minutes, and finally speaking to someone only to get a 30-second update is intensely frustrating. It makes the policyholder feel like a number, not someone you’re there to help. This single point of friction can erase years of brand loyalty.
The Churn Risk is Real
The consequences of a poor claims experience are severe. The claims process is an insurance carrier’s moment of truth. It’s the one time a policyholder interacts with the product they’ve been paying for. A smooth, transparent, and communicative process builds immense loyalty. A frustrating, opaque one is a direct invitation to shop for a new carrier at renewal time.
Studies by firms like J.D. Power consistently show that claims satisfaction is a primary driver of policyholder retention. A customer with an adverse claims experience is multiple times more likely to switch carriers than one with a positive experience. By sticking to a reactive communication model, you are actively pushing your customers into the arms of your competitors. The cost isn’t just the operational expense of the call center; it’s the lifetime value of every policyholder who leaves, dissatisfied with your service.
The Proactive Pivot: A New Era for P&C Claims Management
The solution to the problems of the reactive model is a fundamental shift in mindset: moving from a passive recipient of calls to a proactive provider of information. Proactive communication isn’t just about sending an occasional email; it’s about anticipating your policyholder’s needs and delivering timely, relevant updates at every key milestone of the claims journey.
Think about the modern customer experience in other industries. When you order a package from Amazon, you get notifications when it ships, when it’s out for delivery, and when it arrives. You never have to call and ask, “Where’s my package?” When you order a car from Uber, you see its exact location on a map in real-time. The information comes to you, eliminating uncertainty and building confidence.
This is the new standard of customer service, and the insurance industry is no exception. Policyholders now expect the same level of transparency and communication they receive in every other aspect of their digital lives.
A proactive approach in P&C claims management does several powerful things:
- It closes the Anxiety Gap: You give policyholders peace of mind by providing updates automatically. They know their claim has been received. They know who their adjuster is. They know the inspection is scheduled. This constant flow of information replaces anxiety with confidence and trust. They no longer need to call because their questions are being answered before they can fully form.
- It Sets Clear Expectations: Proactive communication allows you to manage the policyholder’s expectations from day one. An automated call after the First Notice of Loss (FNOL) can explain the next steps and typical timeframes, preventing misunderstandings and frustration. Customers who know what to expect are far more patient and satisfied with the process.
- It Humanizes the Process: This may seem counterintuitive when discussing automation, but it’s true. A well-timed, precise, and empathetic update makes the customer feel seen and valued. It shows that you understand their situation and are actively working on their behalf. It turns an impersonal, bureaucratic process into a supportive journey where they feel guided and informed every step of the way.
The bottom line is that a proactive strategy fundamentally changes the dynamic. You are no longer on the defensive, reacting to customer inquiries. You are in control, leading the conversation, and delivering a superior experience that your policyholders will remember and appreciate.
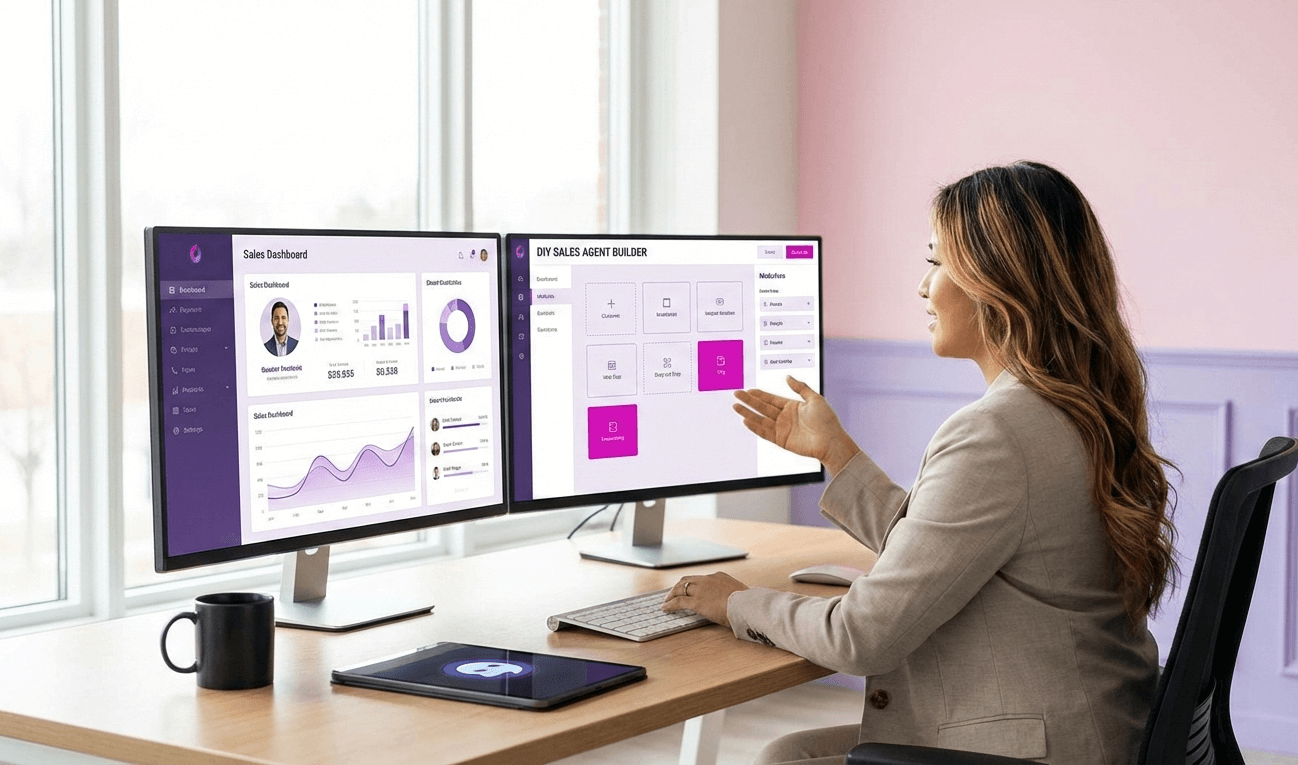
The Engine of Proactivity: The AI Claims Assistant
So, how do you implement a robust, scalable, proactive communication strategy? The answer lies in technology, specifically an AI for insurance claims. This isn’t about a simple chatbot on your website or a clunky Interactive Voice Response (IVR) system. We’re talking about a sophisticated, dedicated AI Claims Assistant that integrates with your core systems and acts as your automated communication engine.
What is an AI Claims Assistant?
An AI Claims Assistant is an artificial intelligence agent designed to handle specific, high-volume communication tasks within the claims workflow. Unlike a general-purpose AI, it is built with a deep understanding of the insurance domain. Its primary function is to monitor your Claims Management System (CMS) for key events and, when one occurs, automatically initiate a proactive, outbound call to the policyholder to provide a clear, concise status update.
How It Works: The Technology in Action
The process is seamless and powerful, a natural extension of your workflow.
- Core System Integration: The AI Claims Assistant connects to your CMS via secure APIs. This is the critical first step. The CMS is the single source of truth for all claim information, from FNOL to final payment. The AI needs to be able to read this data in real-time.
- Event-Based Triggers: You and your team define the key milestones in the claims process that should trigger a communication. These are the moments when a policyholder is most likely to wonder, “What’s next?” Common triggers include:
- Claim Filed (FNOL)
- Adjuster Assigned
- Inspection Scheduled
- Vendor (e.g., body shop, contractor) Assigned
- Estimate Received
- Estimate Approved
- Supplement Approved
- Payment Issued
- Claim Closed
- The Proactive Outbound Call: When a CMS trigger event occurs, an adjuster updates a claim file from “Pending Assignment” to “Adjuster John Smith Assigned.” The AI Claims Assistant is instantly activated. It uses advanced text-to-speech and natural language processing to make a remarkably human call—not like a robot but like a helpful assistant.
- A Clear and Valuable Conversation: The AI delivers a relevant update. “Hi, Mr. Johnson. This is the automated claims assistant from ABC Insurance. I’m calling to give a quick update on your auto claim. I see that adjuster Sarah Bell has just been assigned to your case. She will contact you within 24 business hours to schedule an inspection of your vehicle.”
- Closing the Loop: The call is logged automatically back into the CMS, creating a perfect record of every communication touchpoint. This provides a complete audit trail and ensures your adjusters know precisely what information the policyholder has received.
This insurance claims processing automation system works tirelessly in the background 24/7, ensuring that every policyholder receives the correct information immediately without human intervention.
SalesCloser.ai: Your Dedicated AI Claims Assistant
While the concept of an AI assistant is powerful, the execution is everything. SalesCloser.ai is not a generic AI platform; it is a purpose-built virtual claims adjuster and communication assistant explicitly designed for the unique needs of P&C insurance carriers. It is an insurtech solution built to solve the core problem of reactive communication.
Let’s walk through a real-world scenario to see how SalesCloser.ai transforms the claims experience from the policyholder’s perspective.
A Day in the Life of a Claim with SalesCloser.ai
Meet Maria. A pipe burst in her upstairs bathroom, causing significant water damage to her kitchen ceiling. She’s stressed, displaced, and worried about the repairs. She files her claim through her insurance carrier’s mobile app.
Minute 5: Claim Received (FNOL Automation). Before Maria’s anxiety can even build, her phone rings.
SalesCloser.ai: “Hello, Maria. This is the automated claims assistant calling from Your Insurance Company. We received your new water damage claim, reference number 789-123. We understand this is a difficult time, and our team is already on it. A dedicated adjuster will be assigned and will contact you within the next business day. Thank you for your patience.”
Immediate Impact: Maria’s initial panic subsides. She knows her claim is in the system and the process has started. She doesn’t have to call to confirm. The “anxiety gap” has been prevented before it could even open.
Day 1: Adjuster Assigned. The next morning, a manager assigns the claim to an adjuster named David. This action in the CMS instantly triggers another call.
SalesCloser.ai: “Good morning, Maria. This is a quick update from Your Insurance Company regarding your water damage claim. An adjuster, David Miller, has been assigned to you. His direct number is 555-867-5309. He will call you today to schedule a time to inspect the damage.”
Immediate Impact: Maria now has a name and a number. She feels a personal connection and knows who to expect a call from. She doesn’t have to wonder if anyone is looking at her file. She feels informed and in control.
Day 3: Inspection Scheduled. David called Maria, and they scheduled the inspection for the following day. David updates the CMS with the date and time.
SalesCloser.ai: “Hi Maria, this is a friendly confirmation from Your Insurance Company. Your property inspection with David Miller is scheduled for tomorrow, September 24th, between 10 AM and 12 PM. If you need to reschedule, please contact David directly.”
Immediate Impact: The appointment is confirmed, reducing the chance of miscommunication or a missed appointment that could delay the claim. This simple, professional touch elevates the customer service experience.
Day 5: Estimate Approved & Vendor Engaged. David completed his estimate and approved a reputable water damage restoration company to begin the work. He updates the file in the CMS.
SalesCloser.ai: “Good afternoon, Maria. We have good news regarding your claim. The initial estimate for repairs has been approved. We have engaged First Response Restoration to handle the work, and they will contact you shortly to schedule the start date.”
Immediate Impact: This is a massive moment of relief for Maria. She knows the financial part is approved, and the physical repair process is about to begin. She doesn’t have to call David to ask, “Has the estimate been approved yet?”
Day 10: Payment Issued. Once the work begins, the carrier directly pays the restoration company. The finance department marks “Payment Issued” in the CMS.
SalesCloser.ai: “Hello, Maria. This is an update on claim 789-123. We have issued the first payment directly to First Response Restoration so they can proceed with your repairs. We will keep you updated as your claim progresses.”
Immediate Impact: Maria now has complete transparency into the financial process. This level of proactive communication is unheard of in traditional claims handling and builds trust.
Throughout this process, Maria has not had to make a single outbound call to check on her status. She has been perfectly informed at every critical juncture. She feels cared for, respected, and confident in her insurance carrier. Meanwhile, her adjuster, David, has been able to focus 100% of his time on managing the actual claim—the inspection, the estimate, and vendor coordination—without being interrupted by status-check calls. This is what modern customer service for insurance looks like.
The Ripple Effect: Benefits That Go Beyond the Call Center
The most obvious benefit of implementing a solution like SalesCloser.ai is a drastic reduction in inbound call volume. Our clients typically see a 40-60% or even greater drop in these repetitive status-check calls within the first few months. However, the positive impacts ripple out across the entire organization.
1. Radically Reduced Call Center Costs
This is the most direct ROI. Fewer calls mean you can accomplish more with your existing staff or reduce overhead. The money saved on salaries, training, and telephony infrastructure can be reallocated to other value-adding parts of the business. Automating these simple, high-volume inquiries delivers immediate and measurable financial returns.
2. Empowered and Efficient Adjusters
Your claims adjusters are your most valuable asset in the claims process. They are skilled professionals, not customer service reps. By offloading repetitive communication tasks to an AI assistant, you give them back their most precious resource: time. An adjuster who can focus without interruption on complex problem-solving, negotiation, fraud detection, and settlement finalization is an adjuster who can close claims faster and more accurately. This improves claim outcomes, boosts employee morale, and reduces burnout.
3. Skyrocketing Policyholder Satisfaction
A proactive communication strategy is one of the most effective ways to improve policyholder experience. Customers’ satisfaction (CSAT) and Net Promoter Scores (NPS) soar when they feel informed and respected. This isn’t just a “feel-good” metric. High satisfaction scores are directly correlated with customer loyalty and retention. A happy customer will likely stay with you for years, recommend your company to friends and family, and be more receptive to purchasing additional policies. In a commoditized market, your experience is your most powerful competitive differentiator.
4. Accelerated Claim Cycle Times
Inefficiency has a cascading effect. When adjusters are constantly interrupted, every claim in their queue is delayed. By creating an environment of focused work, automated insurance claim status updates help to speed up the entire process. Faster inspections, quicker estimate approvals, and more timely payments mean that claims move from open to closed in less time. This is a win for everyone: the policyholder gets their life back to normal faster, and the carrier reduces the administrative costs associated with long-running open claims.
5. A Modern, Competitive Edge
Implementing cutting-edge insurtech solutions sends a powerful message to the market. It positions your company as a forward-thinking, customer-centric leader. Today’s consumers, especially younger demographics, expect digital-first, seamless experiences. An AI-powered communication strategy shows that you understand their needs and are invested in using technology to deliver superior service. This can be a deciding factor for potential customers choosing between you and a more old-fashioned competitor.
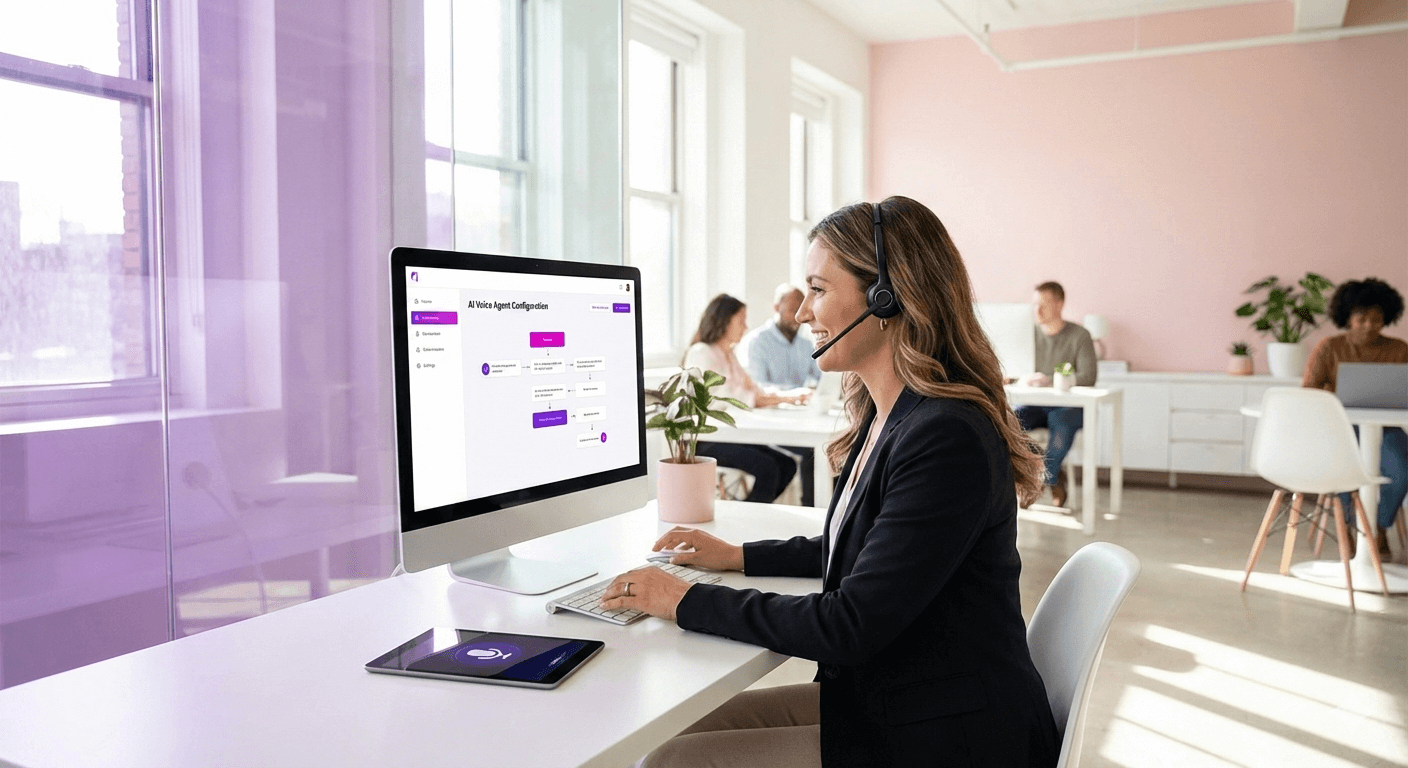
Answering Your Questions: Implementation and Common Concerns
Adopting new technology can feel daunting, but a dedicated solution like SalesCloser.ai is designed for a smooth and straightforward integration. Let’s address some of the most common questions carriers have.
“Will my policyholders be comfortable talking to an AI?” This is a valid concern, but often based on outdated experiences with robotic IVR systems. The conversational AI in SalesCloser.ai is incredibly advanced. Its natural, empathetic tone is programmed for clear, simple communication.
More importantly, consider the alternative. Is a policyholder happier waiting on hold for 20 minutes to talk to a human for a 30-second update, or receiving an instant, proactive call that gives them the exact information they need in under a minute? The value and convenience of the proactive call overwhelmingly lead to a positive reception. It’s not about human vs. AI; it’s about a bad experience vs. a great one.
“How difficult is the implementation process?” SalesCloser.ai is built for integration. Our team works directly with your IT department to establish a secure API connection to your Claims Management System. We help you map out the key trigger points in your specific workflow and customize the call scripts to match your brand’s voice and tone. The collaborative process is designed to minimize the burden on your internal resources. We handle the heavy lifting of the AI and telephony so that you can focus on the results.
“What about data security and compliance?” We understand that we operate in a highly regulated industry where data security is paramount. The SalesCloser.ai platform is built on a secure, compliant foundation, with protocols to protect sensitive policyholder information. We are well-versed in the data privacy and security standards that govern the insurance industry and work with you to ensure all integrations and communications meet those requirements.
It’s Time to Hang Up on the Past
The era of reactive customer service is over. For P&C insurance carriers, continuing to rely on a model where anxious customers must constantly call in for information is no longer operationally or financially sustainable. It’s a model that guarantees high costs, inefficient workflows, and a frustrating policyholder experience.
The future of claims is proactive, transparent, and automated. You can fundamentally change your operational reality by implementing a dedicated AI Claims Assistant to deliver automated insurance claim status updates. You can free your team to focus on what matters most, slash unnecessary costs, and give a claims experience that builds loyalty and sets you apart from the competition.
Stop letting the ringing phone dictate your day. It’s time to take control of the conversation.
Ready to see how SalesCloser.ai can silence your call center and delight your policyholders? Schedule a personalized demo today and witness the future of claims communication.
Frequently Asked Questions (FAQs)
Q1: What exactly is an AI Claims Assistant?
An AI Claims Assistant, like SalesCloser.ai, is a specialized artificial intelligence software designed to automate communication in the insurance claims process. It integrates with your Claims Management System (CMS) to monitor for key events (like an adjuster being assigned or a payment being issued). When these events occur, it automatically calls the policyholder outbound to provide a clear, proactive status update in a natural, human-like voice.
Q2: How does SalesCloser.ai integrate with our existing Claims Management System?
Our system integrates via secure Application Programming Interfaces (APIs). Our implementation team works with your IT staff to connect SalesCloser.ai to your CMS. This allows our platform to read claim data securely in real time to identify the triggers for communication. The process is designed to be lightweight and compatible with most modern claims platforms.
Q3: Can the AI handle complex or emotional customer questions?
SalesCloser.ai is expertly designed for proactive, informational updates. Its primary goal is to deliver clear, accurate information at key milestones to prevent the need for a call in the first place. For simple queries, it can provide answers. However, it is also programmed with intelligent routing. If a policyholder expresses distress, asks a complex question outside the update’s scope, or simply says “I need to speak to a person,” the AI can seamlessly transfer the call to a live agent or the assigned adjuster immediately.
Q4: What kind of Return on Investment (ROI) can we expect?
The ROI is multifaceted. Financially, you’ll see a direct return from a significant reduction in inbound call volume (often 40-60%+), leading to lower call center staffing and operational costs. Operationally, adjuster productivity increases as they spend less time on phone calls and more on core claims work, leading to faster cycle times. From a customer perspective, the improved experience leads to higher CSAT/NPS scores, which are strongly linked to increased policyholder retention and reduced churn.
Q5: How long does it take to get started with SalesCloser.ai?
The implementation timeline can vary depending on the complexity of your CMS and workflows, but a typical rollout can be completed in weeks, not months. Our dedicated onboarding team manages the project from start to finish to ensure a smooth and efficient launch.
Q6: What happens if a policyholder misses the AI’s call?
The system is configurable to your preferences. If a call is unanswered, SalesCloser.ai can be programmed to leave a detailed voicemail with the status update automatically. Additionally, it can trigger a follow-up SMS message or email summarizing the information, ensuring the policyholder receives the critical update through multiple channels.